Medical-Grade Hyaluronic Acid: From Ophthalmic to Multidisciplinary Therapeutic Agent
When people hear of hyaluronic acid (HA), the majority of them will immediately associate it with cosmetic and skincare applications. Whether applied as dermal fillers or as a means to improve skin hydration, HA is indeed highly effective. But the application of HA extends far beyond these.
In general, HA is categorized into different grades based on the application. Besides the usual cosmetic grade, medical-grade, food-grade, and injectable-grade HA also have extensive market applications. We have already touched on the variations between these types of hyaluronic acid. If you’re curious, click on the following link to learn more: Medical Grade vs. Cosmetic Grade Hyaluronic Acid: What Are the Differences.
HA was first discovered to be added to medicine over 70 years ago. It has continued to be a constantly increasing part of life sciences and medicine through continued research.
Medical Grade Hyaluronic Acid Was First Used in Ophthalmology
Hyaluronic acid is a multi-purpose matrix that occurs widely in the human body. It possesses a good lubricant and biocompatibility. Medically, it is referred to as sodium hyaluronate and is utilized in various ophthalmic surgeries, such as intraocular lens implantation, corneal transplantation, and glaucoma surgery.
Actually, the therapeutic application of HA dates back 70 years. HA was first successfully used in eye surgeries in the 1950s and remains a common practice to this day. Two decades later, HA’s moisturizing property was beautifully utilized by veterinarians when they filled horse joints with HA to improve mobility. Since then, HA has steadily expanded its role in medicine.
Read more: From Surgery to Daily Care: The Versatile Role of Sodium Hyaluronate in Eye Health
The Diverse Benefits of Medical-Grade Hyaluronic Acid
Presently, with more and more research, applications of HA in medicine are growing day by day. Besides its traditional use in ophthalmology, HA has become a major treatment modality for orthopedic conditions. In osteoarthritis and frozen shoulder, joint lubrication is greatly improved by HA injections, and cartilage is protected.
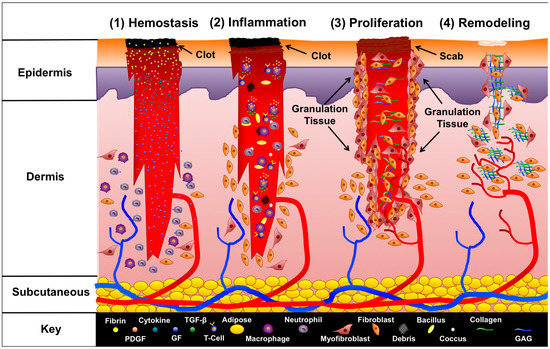
Moreover, HA use now includes gynecology, tendon fixation, and abdominal surgery, wherein it is utilized as a postoperative device. Its bioadhesive nature allows it to form a protective coating over wounds, both as a lubricant and as a mechanical coating to give the optimal environment for healing.[i] Lastly, HA supplementation is now a standard therapy for cystitis and urinary tract infection, significantly alleviating signs and symptoms with its mucosal protective effect.
HA is also pushing vaccine technology forward. By some chemical manipulations, HA holds pioneering promise as an adjuvant. When mixed with antigens, it enhances antigen-presenting efficacy, induces targeted migration to lymph nodes, and prevents inflammation at the injection site[ii]—offering new conceptual paradigms for vaccine design.
The Role of Hyaluronic Acid Depends on Its Molecular Weight
Low-molecular-weight HA (LMW-HA) can penetrate tissues better, possesses fine bioactivity, and is, therefore, good for anti-inflammatory and tissue repair. Medium-molecular-weight HA (MMW-HA) offers a balance between lubrication and structure. High-molecular-weight HA (HMW-HA) excels in viscoelasticity and water retentive properties. Each of the molecular weight forms has something special to offer—no one “best” one, merely the best for a given purpose. Each has a specific molecular weight range suited to a specific medical application and functional requirement.
The next table provides a working comparison of HA’s properties demanded and molecular weight associated for various medical applications:
| Application | Key Performance Requirements | Recommended MW | Mechanism of Action |
| Ophthalmic Surgery | – High viscoelasticity
– Pseudoplasticity – Biocompatibility |
High (1,000–3,000 kDa) | – Maintains anterior chamber space
– Protects corneal endothelial cells – Facilitates surgical instrument maneuverability |
| Joint Injection | – Moderate viscoelasticity
– Long-lasting lubrication – Anti-inflammatory effects |
Medium (500–1,500 kDa) | – Reduces joint friction
– Inhibits pro-inflammatory cytokines (e.g., IL-1β) – Stimulates endogenous HA synthesis |
| Wound Healing | – Tissue permeability
– Cell-activating capacity – Angiogenic promotion |
Low (<50 kDa) | – Activates CD44/TLR4 receptors to promote repair
– Accelerates fibroblast migration – Modulates macrophage polarization |
| Vaccine Adjuvant | – Immune cell targeting
– Enhanced antigen presentation – Low inflammatory response |
Low (10–200 kDa) | – Promotes dendritic cell uptake
– Enhances lymph node targeting – Activates immune response via TLR4 |
| Anti-Adhesion Barrier | – Mechanical separation
– Controlled degradation – Tissue compatibility |
Medium-High (1,000–2,000 kDa) | – Physically isolates wound surfaces
– Degrades slowly (4–6 weeks) – Reduces fibrin deposition |
This structured comparison serves as a reference for clinical decision-making or product development, emphasizing that optimal HA selection depends on specific medical requirements.
[i] Belluco C, Meggiolaro F, Pressato D, Pavesio A, Bigon E, Donà M, Forlin M, Nitti D, Lise M. Prevention of postsurgical adhesions with an autocrosslinked hyaluronan derivative gel. J Surg Res. 2001 Oct;100(2):217-21. doi: 10.1006/jsre.2001.6248. PMID: 11592796.
[ii] Jiang D, Liang J, Noble PW. Hyaluronan as an immune regulator in human diseases. Physiol Rev. 2011 Jan;91(1):221-64. doi: 10.1152/physrev.00052.2009. PMID: 21248167; PMCID: PMC3051404.