When oral intake, Hyaluronic Acid is broken down by intestinal hyaluronidase and gut microbiota into low-molecular-weight fragments. And then HA is absorbed into the bloodstream. Alternatively, Injected HA undergoes localized degradation by hyaluronidases and free radicals, with fragments eventually metabolized or eliminated via the lymphatic system and urine.
Hyaluronic Acid in the Human Body
Hyaluronic acid (hyaluronan, HA) is a naturally occurring polymer that is constantly being synthesized and degraded in the human body. It is found predominantly in the extracellular matrix, vitreous humor, and cartilage. A typical 70 kg adult contains about 15 grams of HA, with about 5 grams metabolized and replaced daily. Surprisingly, nearly half of the whole body's HA can be found within the skin, where its relatively brief half-life is 24 to 48 hours. Owing to its excellent ability to retain moisture, lubricate, and support tissue repair, hyaluronan has been extensively used in dermatology, joint care, and drug delivery systems. Yet, how exactly is HA broken down and absorbed after ingestion or injection?
Absorption Pathways of Hyaluronic Acid
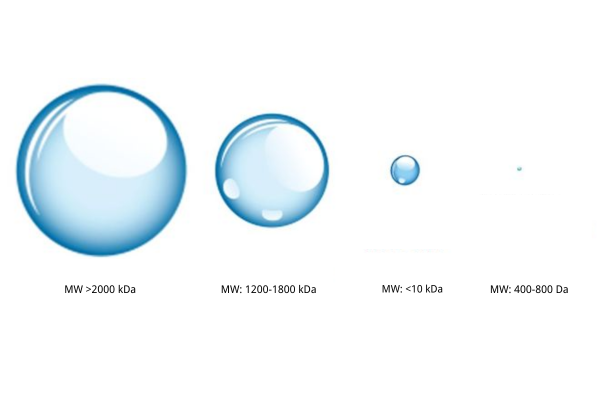
Hyaluronic acid (HA) is a linear polymer that is composed of repeating disaccharide units, and its absorption is also correlated with molecular weight. Research has indicated that low-molecular-weight HA (<50 kDa) would be absorbed by intestinal epithelial cell endocytosis or colonic microbiota degradation. High-molecular-weight HA is degraded by intestinal hyaluronidase to create smaller peptides, which are absorbed into the bloodstream. Oral hyaluronic acid (HA) is primarily broken down in the intestine by enzymes and gut microflora into short molecular fragments, which are absorbed into the bloodstream. These fragments are able to activate skin and joint cells to increase endogenous HA synthesis, resulting in hydration and joint health benefits.
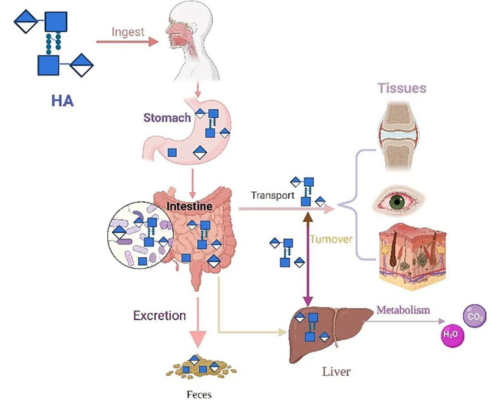
Fig 1. The process of food-grade HA being absorbed by the human body [1] Subcutaneous or intra-articular injection is the most common clinical and medical aesthetic application of HA. As injected HA is deposited inside tissue or fluid in the body, destruction and removal are primarily dependent on local enzymic hydrolysis and lymphatic drainage.
Degradation Mechanisms of Hyaluronic Acid
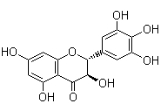
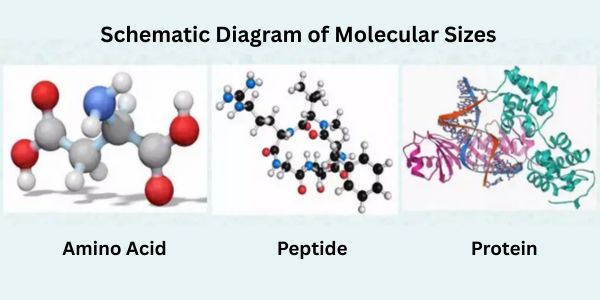
Molecularly, hyaluronic acid consists of two monosaccharides: N-acetylglucosamine and sodium glucuronate (Figure 2). The disaccharide components are connected linearly by β-1,4-glycosidic bonds. Bond cleavage underlies the depolymerization of HA, depending on enzyme activity and free radical degradation. 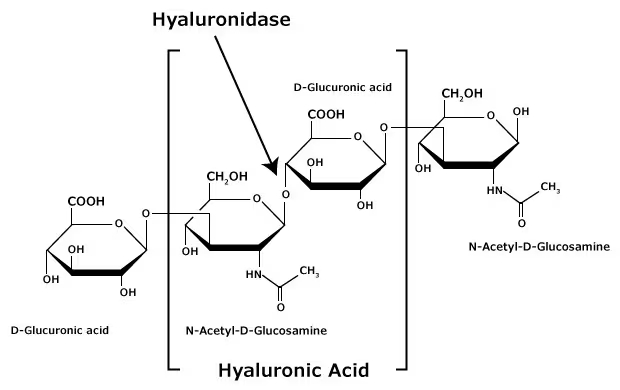
Fig 2. Structure of Hyaluronic Acid
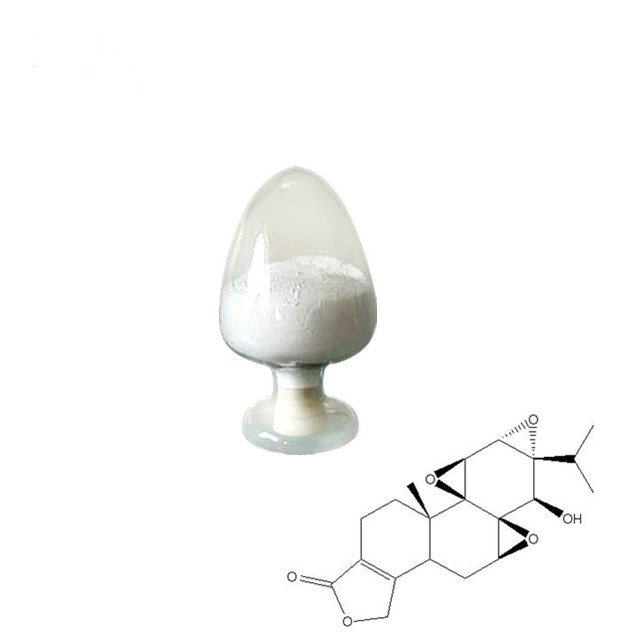
(1) Role of Hyaluronidase
Hyaluronidases (such as HYAL1 and HYAL2) are the primary enzymes responsible for the breakdown of HA. They hydrolyze glycosidic bonds preferentially, breaking down HA to smaller oligosaccharides. They are extensively distributed in tissues like skin, liver, and spleen, so that injected HA will be gradually metabolized and eventually eliminated in urine or further broken down. 
Fig 3. Degradation Pathways of Hyaluronic Acid
(2) Free Radical Degradation
Besides enzymatic degradation, hyaluronic acid is also degraded by oxidative stress resulting from reactive oxygen species (ROS) and other free radicals. Oxidative stress increases in inflamed or aged tissues, where glycosidic bond cleavage through ROS occurs frequently.
(3) Factors Influencing HA Degradation Rate
The rate at which HA breaks down in the body depends on several key factors:
- Molecular weight: High-molecular-weight HA degrades more slowly than its low-MW counterpart.
- Crosslinking: Chemically crosslinked HA (e.g., in dermal fillers) resists enzymatic breakdown, extending its longevity.
- Injection site: Areas with high blood flow (e.g., lips) metabolize HA faster than low-circulation regions (e.g., joints).
- Individual variability: Age, metabolic rate, and natural hyaluronidase levels all influence degradation speed.
Why Does the Skin Need Hyaluronan Supplementation?
Hyaluronan turnover in the skin is a quiet balance between synthesis and degradation. HA is synthesized by mesenchymal cells via the activity of hyaluronic acid synthases (HAS-1, HAS-2, HAS-3) and is degraded simultaneously by hyaluronidases. With time, this equilibrium is disturbed—degradation is greater than synthesis, leading to a decrease of HA. To offset this deficit, topical HA skin-care products and injectable dermal fillers are used to restore missing HA and rehydrate and structurally maintain aging skin. Stanford Chemicals Company (SCC) is a supplier with over 10 years of expertise in hyaluronic acid. If you'd like to learn more about hyaluronic acid or are interested in purchasing sodium hyaluronate powder, please feel free to contact us.
FAQs
- How does the body absorb hyaluronic acid?
Only the low molecular weight HA molecules (below 50 kDa) are absorbed when taken orally, whereas larger molecules are broken down first. Injected HA stays put until it is slowly broken down by enzymes.
- What breaks down hyaluronic acid in the body?
Special enzymes called hyaluronidases break down HA naturally. The enzymes cut the HA molecules into pieces that the body can either reuse or eliminate. Active oxygen molecules are also capable of breaking down HA faster, especially in older or inflamed tissue.
- Why does injected HA persist longer than topical HA?
Injected HA forms a depot under the skin that lasts a long time to weeks to months to be metabolized. Topical HA is only able to penetrate as far as the surface layers and is removed or degraded much faster since it doesn't deeply penetrate.
- Why does HA degrade more rapidly?
HA is degraded faster in highly mobile tissues (like lips), in younger people who possess more active enzymes, and in inflamed tissue in where oxygen radicals and enzymes increase. Crosslinked HA, which is used in fillers, breaks down more slowly than native HA.
- Do you slow the degradation of HA?
Yes. Avoiding excessive sun exposure, avoiding smoking, and using antioxidants (like vitamin C) can safeguard HA.
- Why do we need to replace HA as we age?
Our own bodies make less HA and degrade it more rapidly after about age 25. This causes drying skin and crunchier joints. HA added to treatments or skincare replenishes this natural loss.
- Is broken-down HA poisonous?
No. The body either recycles the small pieces of HA or simply expels them harmlessly. Yes. Exercise in moderation increases HA production in joints, but extremely intense exercise can increase inflammation and HA breakdown in the short term.